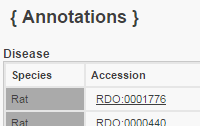
Gene Ontology Annotations Click to see Annotation Detail View
Biological Process Object Symbol | Species | Term | Qualifier | Evidence | With | Notes | Source | Original Reference(s) | Tgfb1 | Rat | positive regulation of collagen biosynthetic process | | IMP | | | RGD | | Tgfb1 | Rat | positive regulation of mononuclear cell migration | | IMP | | | RGD | | | |||||||||||||||||
|
|