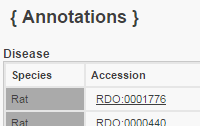
Phenotype Annotations Click to see Annotation Detail View
Mammalian PhenotypeTerm | Qualifier | Evidence | With | Reference | Notes | Source | Original Reference(s) | abnormal circulating chemokine level | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | abnormal circulating myoglobin level | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | abnormal nitric oxide homeostasis | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased cardiomyocyte apoptosis | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased circulating lactate dehydrogenase level | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased circulating troponin level | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased circulating tumor necrosis factor level | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased interleukin-1 beta secretion | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased left ventricle systolic pressure | | IMP | | 126925167; 126925167; 126925167 | | RGD | | decreased macrophage cell number | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | decreased ventricle muscle contractility | | IMP | | 126925167; 126925167; 126925167 | | RGD | | increased cardiac muscle contractility | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | increased circulating lactate dehydrogenase level | | IMP | | 126925167; 126925167; 126925167 | | RGD | | increased circulating myoglobin level | | IMP | | 126925167; 126925167; 126925167 | | RGD | | increased circulating troponin level | | IMP | | 126925167; 126925167; 126925167 | | RGD | | increased left ventricle systolic pressure | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | oxidative stress | | IMP | | 126925167; 126925167; 126925167 | compared to Wild Type in cardiopulmonary bypass model | RGD | | | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|